
04 Mar WHAT ARE THE MOST COMMON ALLERGIES THAT ALLERGEX NON-DROWSY IS PRESCRIBED FOR?
Allergex Non-Drowsy contains Loratadine, a long lasting antihistamine 1,2 1
that is typically prescribed for the relief of symptoms associated with allergic rhinitis such as rhinorrhoea, itchy nose and throat.1,2
It is also indicated to alleviate symptoms of allergic skin reactions and hives.1,2 Let’s take a closer look at what some of these conditions entail. 1
Rhinitis
Simply put, symptoms of rhinitis could include a runny, itchy or stuffy nose, due to blockage or congestion and it can also cause sneezing. ³ 2
This can either be caused by an allergy or a multitude of other factors. 3 2
In the case of rhinitis, the nose usually produces mucus which traps elements such as pollen, germs, dust or bacteria, to name but a few. The mucus flows from the front of the nose to the back of the throat so that it can drain. When excessive or thick mucus is produced, it can cause a post-nasal drip which in turn, will cause you to cough, to clear the throat.³ 2
In summary, rhinitis presents as a runny, itchy or stuffy nose that can be caused by an allergy or other factors. It could cause you to sneeze and produce mucus, which can in turn become thick and excessive and cause a post-nasal drip or a cough.³ 2
Rhinorrhoea
Most commonly referred to as a runny nose, rhinorrhoea is caused by an excess of fluid or mucus that drains from the nose, intermittently or constantly. This fluid can be clear or cloudy, and thick or thin. ⁴ 3
Rhinorrhoea can be caused by a myriad of different factors, including allergic rhinitis, such as described above, which is basically a nasal reaction to allergens such as pet dander or pollen. ⁴ 3
Hives
Hives can either be red, swollen patches or red spots that sting or burn and can appear anywhere on the skin of both children and adults.5 4
Hives typically occur because of triggers that cause a release of high levels of histamine or other chemicals in the skin. These triggers can include a variety of elements such as pollen, plants, insect bites and stings, food and chemicals, to name but a few. 5 4
Dosage and usage of Allergex Non-Drowsy
Generally, the dosage of Allergex Non-Drowsy is prescribed as follows:
- Children two to five years of age: five ml (one medicine measure) of Allergex Non-Drowsy Syrup, once daily¹
- Children six to twelve years of age and over: ten ml (two medicine measures) of Allergex Non-Drowsy Syrup once daily¹
- Adults and children twelve years and over: ten ml (two medicine measures) of Allergex Non-Drowsy Syrup. ¹
- One Allergex Non-Drowsy tablet, once daily. 2 1
There are however a multitude of factors that could affect the usage and efficacy of antihistamine such as Allergex Non-Drowsy, which includes chronic or other medical conditions and use of other medicines. It is therefore critical to consult with your doctor or pharmacist first.
References:
- Allergex Non-Drowsy Syrup approved package insert, January 2003.
- Allergex Non-Drowsy Tablets approved package insert, January 2004.
- St Joseph Hospital, a member of the St. Joseph Hoag Health Alliance. What is rhinitis? Accessed on 16 November 2018. Available at: https://www.sjo.org/our-services/nasal-sinus-center/allergies/what-is-rhinitis-/
- Stanford’s Children’s Health, Lucille Packard Children’s Hospital, Stanford. Chronic rhinorrhoea (Runny nose). Accessed on 16 November 2018. Available at: https://www.stanfordchildrens.org/en/service/ear-nose-throat/conditions/chronic-rhinorrhea
- National Health (NHS) UK. Reviewed on 6 February 2018. Accessed on 16 November 2018. Available at: https://www.nhs.uk/conditions/hives/
S1 Allergex® Non Drowsy Tablets. Each tablet contains loratadine 10 mg. Reg. No. 36/5.7.1/0286
S1 Allergex® Non Drowsy Syrup. Each 5 ml contains loratadine 5 mg. Reg. No. 36/5.7.1/0008
For full prescribing information, refer to the package insert approved by the medicines regulatory authority. 2018112810111292
Adcock Ingrams Limited. Reg. No. 1949/03485/06. Private Bag X69, Bryanston, 2021, South Africa.
Tel. +27 11 635 0000, www.adcock.com.
BIBLIOGRAPHY AND SOURCES
- Adcock Ingram. Allergex Non-Drowsy. Accessed on 16 November 2018. Available at: adcockingram.co.za/products
Allergex Non-Drowsy is used for the relief of symptoms associated with allergic rhinitis such as sneezing, rhinorrhea (runny nose), and itching of the nose and throat. Is also indicated for the relief of chronic idiopathic urticaria (hives) and other allergic dermatoses (allergic skin reactions). 1
- Allergex Non-Drowsy contains Loratadine.
- Loratadine is a long acting antihistamine, that only needs to be taken once daily 1
Dosage:
- Children 2 to 5 years of age:5 ml (1 medicine measure) once daily
- Children 6 to 12 years of age:10 ml (2 medicine measures) once daily
- Adults and children over 12 years of age:10 ml (2 medicine measures) or 1 tablet once daily 1C
Available in the following packs and formats:
- Allergex ND Syrup 150ml
- Allergex ND Tablets 10s
- Allergex ND Tablets 30s
Available at most leading pharmacies
2. St Joseph Hospital, a member of the St. Joseph Hoag Health Alliance. What is rhinitis? Accessed on 16 November 2018. Available at: https://www.sjo.org/our-services/nasal-sinus-center/allergies/what-is-rhinitis-/
WHAT IS RHINITIS?
Rhinitis is a term describing the symptoms produced by nasal irritation or inflammation. Symptoms of rhinitis include runny nose, itching, sneezing and stuffy nose due to blockage or congestion. 2
These symptoms are the nose’s natural response to inflammation and irritation. Arbitrarily, rhinitis lasting less than six weeks is called acute rhinitis, and persistent symptoms are called chronic rhinitis. Acute rhinitis is usually caused by infections or chemical irritation. Chronic rhinitis may be caused by allergy or a variety of other factors. 2
The nose normally produces mucus, which traps substances like dust, pollen, pollution, and germs such as bacteria and viruses. Mucus flows from the front of the nose and drains down the back of the throat, but when mucus production is excessive, it can flow from the front, as a runny nose, or become noticeable from the back, as post-nasal drip. Nasal mucus, normally a thin, clear liquid, can become thick or colored, perhaps due to dryness, infection or pollution. When post-nasal drip is excessive, thick, or contains irritating substances, cough is the natural response for clearing the throat. 2
Itching and sneezing are also natural responses to irritation caused by allergic reactions, chemical exposures (including cigarette smoke), temperature changes, infections and other factors.
The nasal tissues congest and decongest periodically. In most people, nasal congestion switches back and forth from one side to side of the nose to the other in cycles several hours long. Some people, especially those with narrow nasal passages, notice this nasal cycle more than others. Strenuous exercise or changes in head position can affect nasal congestion. Severe congestion can result in facial pressure and pain, as well as dark circles under the eyes.
3. Stanford’s Children’s Health, Lucille Packard Children’s Hospital, Stanford. Chronic rhinorrhoea (Runny nose). Accessed on 16 November 2018. Available at: https://www.stanfordchildrens.org/en/service/ear-nose-throat/conditions/chronic-rhinorrhea
Chronic rhinorrhea (Runny nose)
What is rhinorrhea or runny nose
Rhinorrhea, or a runny nose, happens when excess fluid drains from the nose. The fluid is mucus that is thin or thick, clear or opaque, and can be intermittent or constant. 3
What causes rhinorrhea?
The nose and sinuses normally produce mucus which keeps the nose moist and is typically swept back into the throat and swallowed. There are many conditions that can cause the nose to run, including:
- Colds and flus: Mucus from illnesses can fill the nasal cavity and cause temporary nasal obstruction.
- Crying: When you cry, tears drain through the tear ducts, into the nasal cavity, and then into the nose.
- Cold Weather: Cold weather can sometimes cause a reaction that produces mucus.
- Infections of the sinuses and or adenoids: The sinuses, or cavities of the face that drain into the nose, can fill with infected mucus resulting in sinusitis (inflammation of the sinuses). The adenoids, tissue found in the back of the nose (nasopharynx), in children can also get infected and result in a similar production of infected mucus.
- Allergic rhinitis: Mucus can result from allergies, or a nasal reaction to allergens such as pollen or pet dander. 3
- Non-allergic rhinitis: Mucus can result from a nasal reaction to an irritant like smoke or pollution, or the body’s reaction to other stimuli like cold weather or hot food.
- Large/swollen turbinates: The bones along the inside the nose (turbinates) can swell due to allergies or infections and result in nasal obstruction.
- Large adenoids: When the tissue in the back of the nose in children is enlarged.
- Nasal polyps: Grape-like growths in the lining of the nose.
- Foreign body insertion: Often in younger children, the cause of obstruction may be the placement of an object in the nose, such as a peanut or a bead, causing obstruction, and foul smelling mucus drainage.
- Nasal cysts or tumors: Rarely, obstruction is from benign or malignant tumors, or cysts, more commonly seen when the symptoms affect only one side of the nose.
- Choanal atresia or piriform aperature stenosis: Choanal atresia describes the situation when the back of the nose (nasopharynx), is closed off with bone and/or tissue at birth. When this is present on both sides (bilateral), it is often found right after birth. However, if it is only present on one side, it is often not discovered until later in life. Piriform aperature stenosis describes when the bony nasal opening is narrow, obstructing the nose.
- Deviated nasal septum: The right and left sides of the nose are separated by a wall made of bone and cartilage called the nasal septum. At times, the septum can lean more to one side, causing an obstruction on that side. This deformity can be present at birth or a result of trauma to the nose later in life.
Why is rhinorrhea a concern?
Often, rhinorrhea goes away on its own. When it persists or lasts longer than 10 days, a runny nose can be a sign of other conditions, such as those listed above. If a high fever is present, consult your doctor.
How do we evaluate it?
When a runny nose is persistent, your child may be asked to see an allergist by your primary care doctor. Your child may also be asked to see an Ear, Nose and Throat specialist (Otolaryngologist). The specialist will get a complete history and examine the front of the nose, and just along the inside. A speculum may be used for a better view of the nose, and in some cases, a flexible fiberoptic camera may be used to evaluate the entire nasal cavity to the very back of the nose (nasopharynx). This can be done in the clinic without the need for general anesthesia.
How is rhinorrhea treated?
Once the source of the runny nose is found, treatment can include watchful waiting, washing the nose with nasal rinses, medications taken by mouth or sprayed into the nose, or even surgery.
What are the long-term effects of rhinorrhea?
Depending on the source of the runny nose, the long-term effects can vary. Nasal irritation and nasal obstruction can impact a child’s quality of life if it is longstanding. An obstructed nasal passageway can affect sleep quality. Breathing from the nose is also important for facial development in childhood. Rarely, acute infections of the sinuses can lead to more serious infections if left untreated. Nasal obstruction and rhinorrhea may impact the health of the ears and hearing as the drainage pathway for the middle ear is through the back of the nose (nasopharynx).
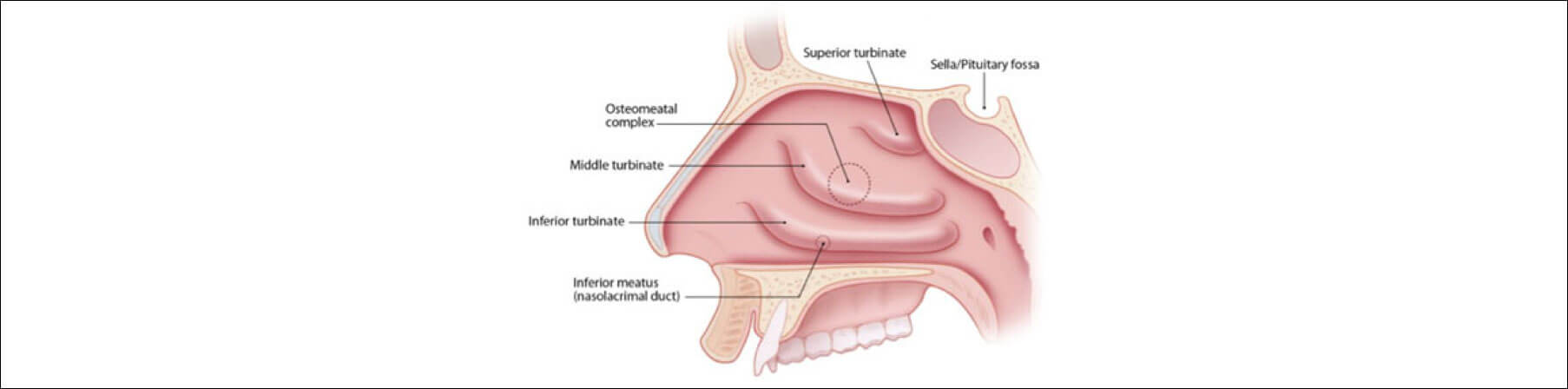
Side view of the nasal cavity showing the bony structures inside the nose.
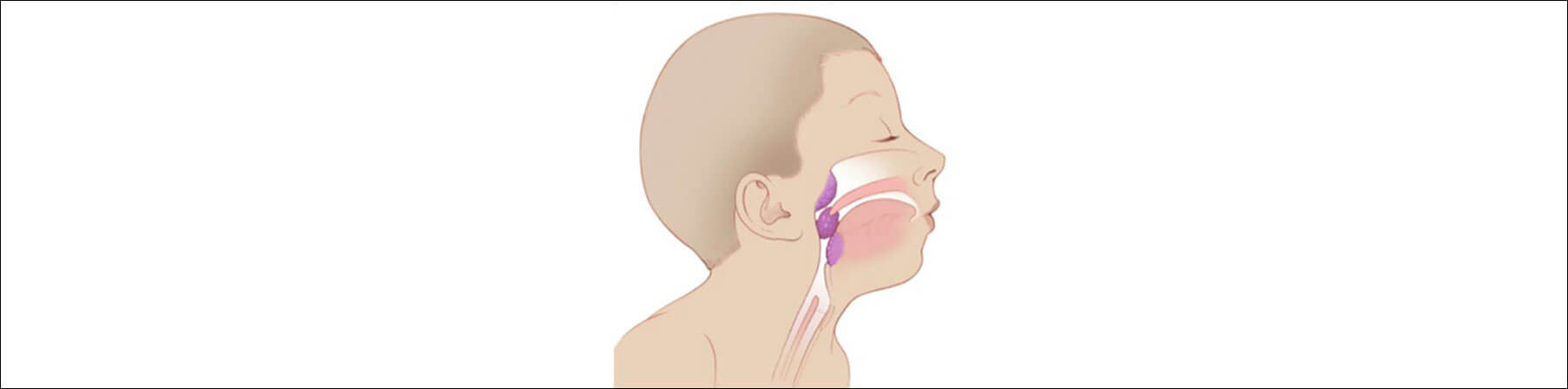
Side view showing where adenoids lay in the back of the nose (nasopharynx). Adenoids are made of the same type of tissue, called lymphoid tissue, as the tonsils in the throat. This tissue can also be found in the back of the tongue, called lingual tonsil.
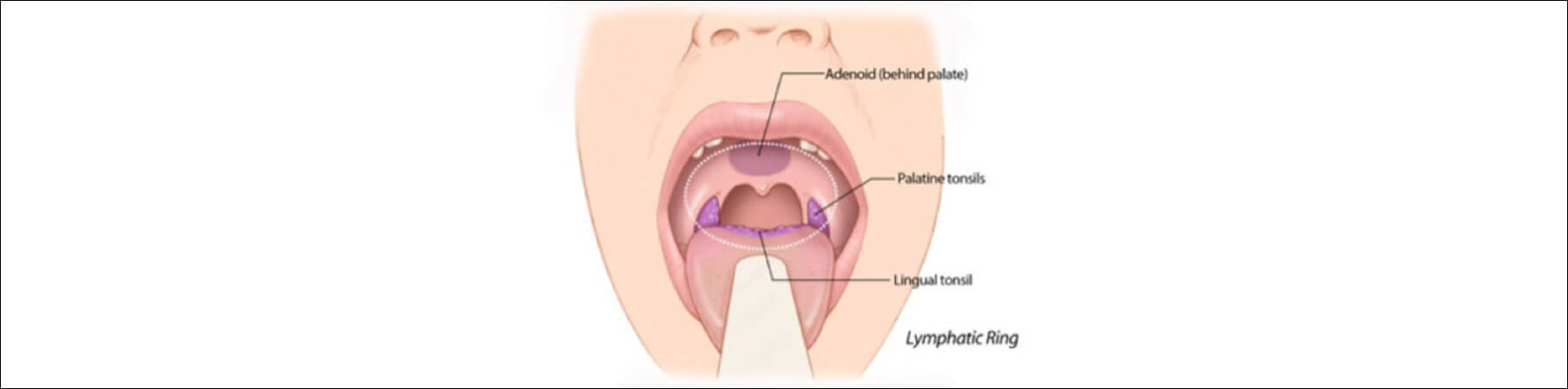
Front view showing where adenoids are in the back of the nose, just above the mouth palate. The back of the nose drains into the back of the throat. This picture also demonstrates how these parts work together, in what is often called a “lymphatic ring”.
Learn more about Pediatric Otolaryngology or call us at (650) 724-4800 for more information.
4. National Health Service (NHS) UK. Reviewed on 6 February 2018. Accessed on 16 November 2018. Available at: https://www.nhs.uk/conditions/hives/
Hives
Hives rashes usually settle down within a few minutes to a few days. You can often treat hives yourself.
Check if you have hives
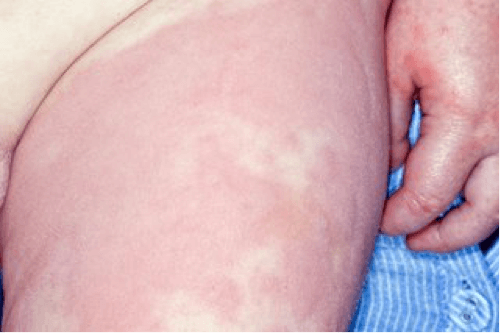
Hives can look like red, raised patches.

The rash can also be red spots
Hives can be different sizes and shapes, and appear anywhere on the body in both adults and children.
The rash is often itchy and sometimes feels like it’s stinging or burning. 4
If you’re not sure it’s hives
Look at other rashes in babies and children.
A pharmacist can help with hives
Your pharmacist can give you advice about antihistamine tablets to bring down your hives rash.
Tell your pharmacist if you have a long-term condition – you might not be able to take antihistamines.
They also may not be suitable for young children.
They also may not be suitable for young children.
See a GP if:
- the symptoms don’t improve after 2 days
- you’re worried about your child’s hives
- the rash is spreading
- your hives keep coming back – you may be allergic to something
- you also have a high temperature and feel generally unwell
- you also have swelling under the skin – this might be angioedema
Go to A&E or call 999 if you have:
- difficulty breathing
- difficulty swallowing
- dizziness or fainting
- nausea or vomiting
- an increased heart rate
- rapid and severe swelling of the face, mouth or throat
These could be signs of a severe allergic reaction, such as anaphylactic shock.
Treatment from a GP
Your GP may prescribe corticosteroids, menthol cream or stronger antihistamines.
If your hives don’t go away with treatment, you may be referred to a skin specialist (dermatologist).
You can’t always prevent hives
Hives occur when something causes high levels of histamine and other chemicals to be released in the skin. This is known as a trigger.
Triggers can include:
- food
- pollen and plants
- insect bites and stings
- chemicals
- latex
- dust mites
- heat – work and sleep in a cool room and wear loose, lightweight clothes
- sunlight, exercise or water
- medicines – speak to your GP if you have an allergic reaction
- infections
- emotional stress 4
Page last reviewed: 06/02/2018
Next review due: 06/02/2021

